A bursa is a small fluid-filled sac bounded by synovial membrane having an inner capillary layer of viscous synovial fluid. They are located over the joints and bony protuberances and may or may not interact with the joint. They decrease friction and protect the fragile structures from stress.
Structure
There are two types of bursae, one that is normally present and second, an adventitious bursa, which develops due to trauma, friction, pressure, etc. The lack of true endothelial or synovial lining makes adventitious bursa various from true bursa. When subjected to repeated pressure, they give rise to bursitis.
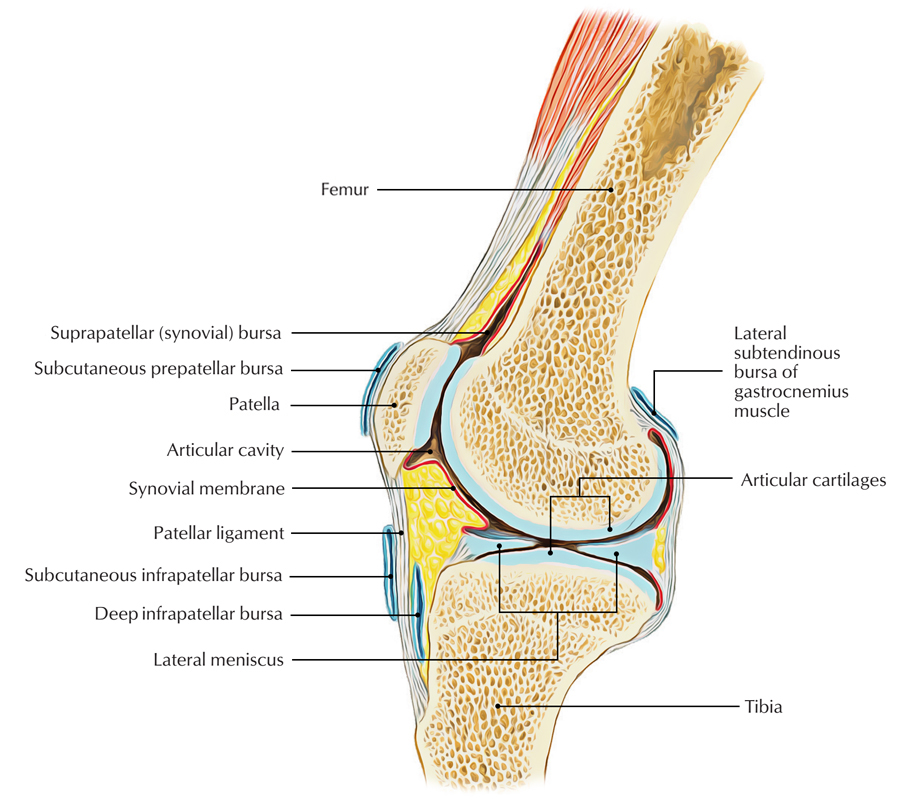
Knee Bursae
Several bursae surround the knee:
- Anteriorly:
- Suprapatellar bursa
- Subcutaneous prepatellar bursa
- Deep infrapatellar bursa and
- Subcutaneous infrapatellar bursa
- Posterolaterally:
- Lateral gastrocnemius.
- Biceps femoris in between the muscle tendon and the fibular collateral ligament.
- The popliteus bursa a.k.a. bursa of the popliteus tendon in between the muscle tendon and the lateral femoral condyle.
- Posteromedially:
- Medial gastrocnemius – semimembranosus bursa in between the medial head of gastrocnemius and the tendon of semimembranosus
- Deep to the medial collateral ligament and in between the tendons of semimembranosus and semitendinosus further variable bursae may be found
Functions
- To prevent friction between two structures that is liable to be rubbed against each other like tendons and bones
- To avoid wear and tear of muscles and tendons
- To protect the frameworks from pressure and injury
Clinical Significance
Baker’s Cyst
It is a swollen bursa emerging from any one of the structures below but the precise origin is not known.
- Between hamstrings and collateral ligaments
- Between hamstrings and tibial condyles
- Each head of gastrocnemius
Symptoms are seen commonly in bursa of the medial head of gastrocnemius and semi-membranosus bursa.
Occurrence
- In 30 percent of cases, herniation of synovial membrane appears through posterior part of capsule.
- Escape of fluid through the normal connection of bursa with knee is the other level of this condition, via either semi-membranosus or medial gastrocnemius.
- Site is undetermined or random in about 10 percent of situations.
Medial Gastrocnemius Bursitis
If the medial gastrocnemius bursa is involved, a palpable mass shows up in between the medial head of the muscle and the semimembranosus tendon and is located in the midline of the popliteal space or extends beneath the head of the gastrocnemius, simulating an enlarged semimembranosus bursa.
In the latter instance, semimembranosus bursitis when in the midline of the popliteal space, when it comes to the bursa is cut off through a posteromedial incision after arthroscopy with the patient supine, it is excised surgically.
Bursitis
- Description: Inflammation of any of different bursae around knee, evidenced by swelling and/or pain; generally prepatellar bursa, pes anserinus bursa, tibial collateral ligament bursa, deep infrapatellar bursa.
- Mechanisms of injury: Usually overuse and may be because of direct blow with bleeding into bursa.
- Predisposing elements: For pes anserinus bursitis, tight hamstrings seem to incline.
- Presentation:
- Issues of swelling, if it is prepatellar bursa.
- Pain in prepatellar region for prepatellar bursitis.
- Pain in distal patellar tendon region for deep infrapatellar bursitis.
- Pain in proximal medial tibia or pes anscrinus bursitis.
- Pain over medial joint line for tibial collateral ligament bursitis.
- Examination: For prepatellar bursa, look for localized swelling and tenderness; for others, tenderness over specific areas.
- Differential medical diagnosis:
- For deep infrapatellar bursitis.
- Other reasons for patellar tendon pain.
- For tibial collateral ligament bursitis, medial meniscus tears.
- For prepatellar bursitis, usually no differential.
- For pes anscrinus bursitis, pain from pes anscrinus tendons, tumors, other reasons for proximal medial tibial pain.
Treatment
- Acute prepatellar bursitis: ice, compression, possible aspiration, padding.
- Chronic prepatellar bursitis: NSAIDs, compression, hamstring extending, ultrasound, and corticosteroid injection.
- Pesanscrinus bursitis: hamstring stretching, ultrasound, NSAIDs, corticosteroid injection.
- Tibial collateral ligament bursitis: injection, both as diagnostic test and as therapy.
- Deep infrapatellar bursitis: hamstring extending, possible injection behind patellar tendon

 (50 votes, average: 4.82 out of 5)
(50 votes, average: 4.82 out of 5)