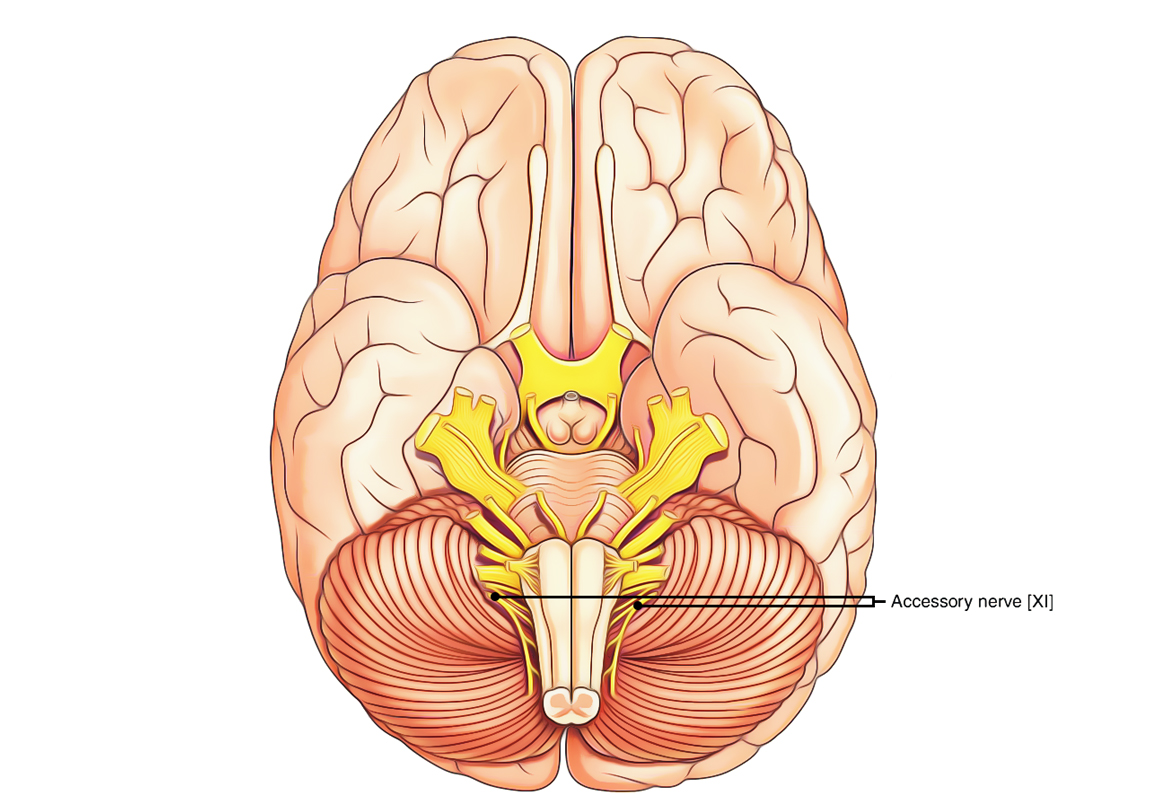
Accessory nerve is the 11th cranial nerve and has motor functions only. It is composed of 2 roots, cranial and spinal. The cranial root is accessory to the vagus and its fibres are dispersed via the vagus nerve. The spinal root has a separate course and is normally regarded as spinal accessory nerve, or merely as accessory nerve.
Accessory Nerve
Functional Elements and Nuclei
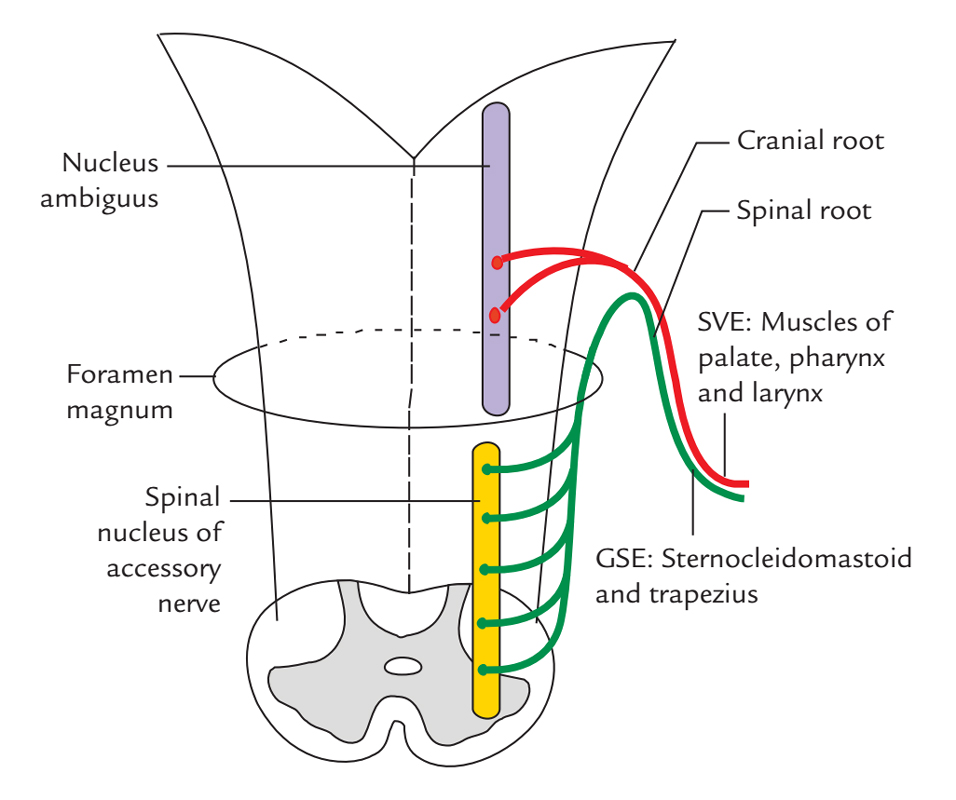
Accessory Nerve: Fucntional Elements and Nuclei
Special visceral efferent fibres: They originate from the nucleus ambiguus and create the cranial root. They give motor supply to the muscles of soft palate, pharynx and larynx. General somatic efferent fibres: They give motor supply to the sternocleidomastoid and trapezius muscles. They originate from the spinal nucleus of accessory nerve, in the ventral horns of the upper 5 spinal sections and create the spinal root.
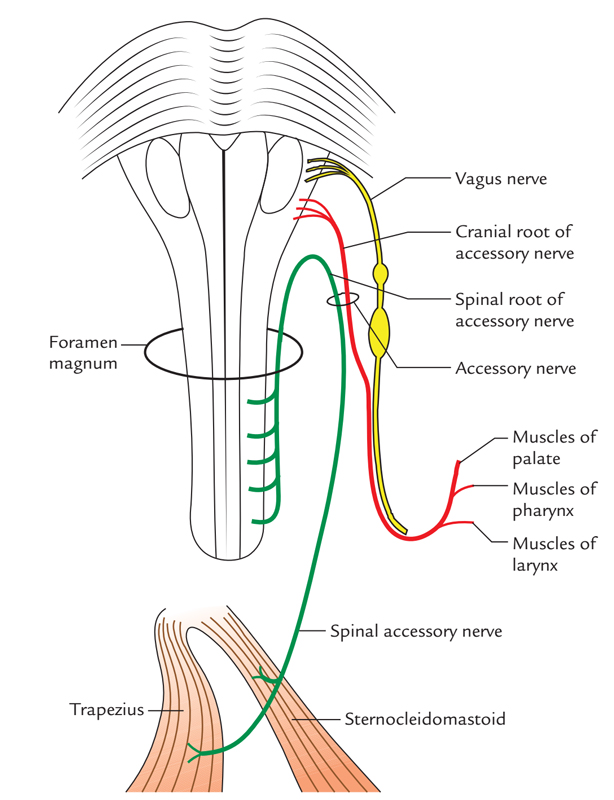
Course and Connections of Accessory Nerve
- From the posterolateral sulcus of the medulla between the olive and inferior cerebellar peduncle the cranial root originates by three or four rootlets. The rootlets are connected in keeping with the rootlets of the vagus nerve above. These rootlets unify together to create one trunk which runs laterally together with the 9th and 10th cranial nerves to reach the jugular foramen where it’s joined by the spinal root.
- The spinal root originates by a number of rootlets from the lateral aspect of the spinal cord (upper 5 cervical spinal sections) along a vertical line between the ventral and dorsal roots of the spinal nerves. These rootlets unify to create an individual trunk which ascends in the vertebral canal to goes into the cranial cavity via the foramen magnum behind the vertebral artery.
- The spinal root leaves the skull via the jugular foramen where it fuses with the whole cranial root. The combined trunk comes out of the cranial cavity via the middle compartment of the jugular foramen enclosed in the dural sheath together with the vagus nerve.
- Promptly after coming out of the cranial cavity, both roots again independent. The cranial root joins the vagus nerve just below its inferior ganglion and is dispersed via the branches of the vagus to the muscles of the palate, pharynx and larynx.
- The spinal root of the accessory nerve descends vertically downward between the internal jugular vein and the internal carotid artery. As it reaches a point midway between the angle of the mandible and the mastoid process, it turns downward and backwards across (superficial or deep) the internal jugular vein toward the carotid triangle. It crosses in front of the transverse process of the atlas under the posterior belly of the digastric muscle and occipital artery. Here it’s escorted by the upper sternomastoid branch of the occipital artery.
- The nerve pierces the sternocleidomastoid muscle in the junction of its upper quarter with the lower three-fourth and supplies it. The nerve goes through the muscle and issues via its posterior border a little above its middle to goes into the posterior triangle where it runs downward and backward underneath the fascial roof of the posterior triangle, parallel to the fibres of levator scapulae.
- It leaves the posterior triangle by passing deep to the anterior border of the trapezius about 5 cm above the clavicle.
- The spinal accessory nerve interacts with the C2, C3 and C4 spinal nerves. The C2 and C3 spinal nerves carry proprioceptive fibres from the sternocleidomastoid while C3 and C4 carry proprioceptive fibres from the trapezius muscle
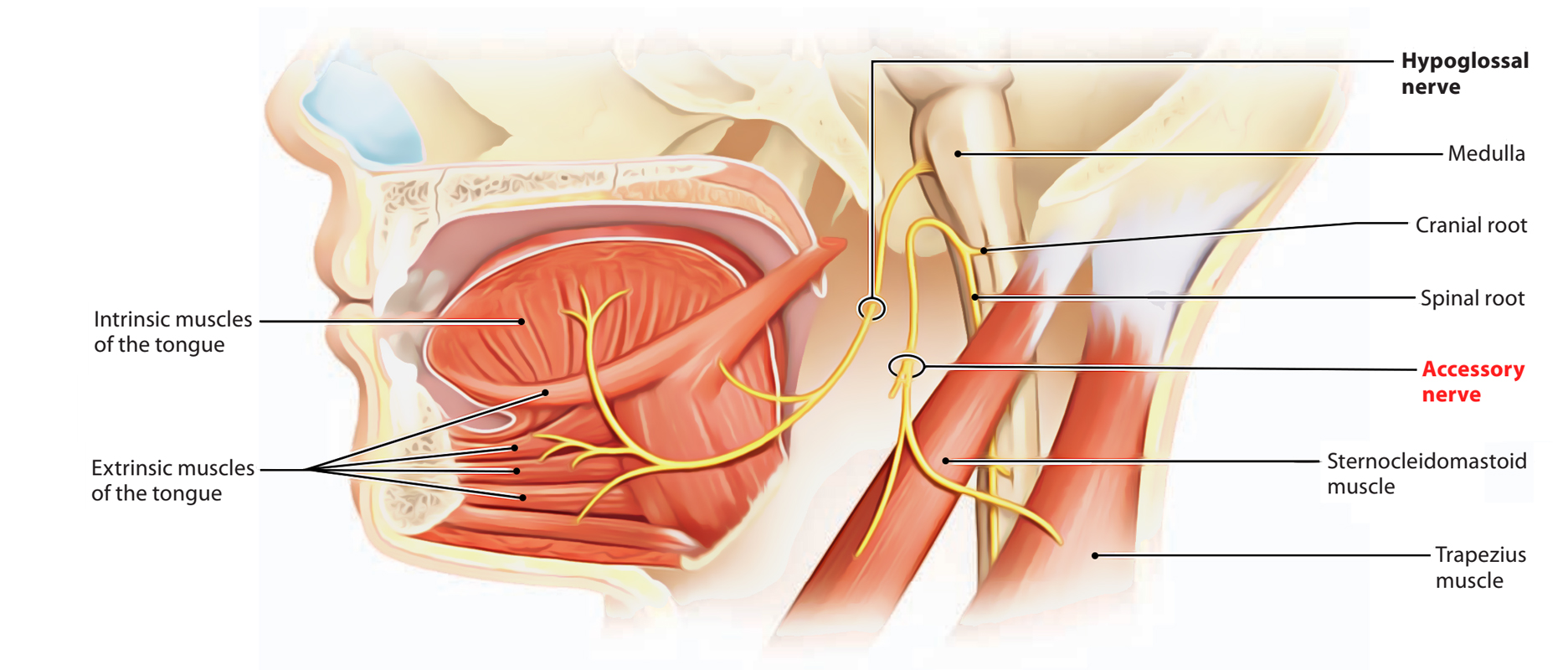
Distribution of Accessory Nerve
Accessory Nerve: Distribution
The cranial root of the accessory nerve through the vagus nerve and pharyngeal plexus of nerves supplies: All the muscles of the palate with the exception of the tensor palati and tensor tympani that are supplied by the mandibular nerve (nerve to medial pterygoid):
- All the muscles of the pharynx with the exception of the stylopharyngeus that is supplied by the glossopharyngeal nerve.
- All the intrinsic muscles of larynx.
- The spinal root of the accessory Nerve Supplies the following 2 muscles:
- Sternocleidomastoid muscle together with C2 and C3 spinal nerves.
- Trapezius muscle together with C3 and C4 spinal nerves.
Functions of Accessory Nerve
The major function of the accessory nerve the motor innervation of the sternocleidomastoid and trapezius muscles.
- The sternocleidomastoidacts in elevation of the thoracic cage and shoulder girdle, or, with fixation of the limb, will act in lateral flexion of the head to the shoulder on the same side and rotate the head to direct the chin upward to the opposite side.
- The trapeziusmuscle is among the muscles that elevate the shoulder girdle and retract the girdle dorsally.
Accessory Nerve Injury
Injury to the accessory nerve can be clinically presented as:
- Shoulders develop the inability to shrug because the trapezius muscle gets paralyzed.
- Head rotation becomes really difficult due to paralysis of the sternocleidomastoid muscle.
Clinical Significance
Lesions of Spinal Accessory Nerve
It might be damaged by the fracture base of the skull via the jugular foramen or stab wounds in the neck or during the surgical removal of cervical lymph nodes. Unilateral/lesion of the spinal accessory nerve proximal to sternocleidomastoid causes:
- Ipsilateral paralysis of the sternocleidomastoid, together with the effect the patient is not able to tip his head toward the ipsilateral shoulder and unable to turn his face toward the opposite side,
- Paralysis of trapezius, together with the consequence the patient is not able to shrug his shoulder against the resistance.
- Spasmodic torticollis: It might result from irritative central lesions of the spinal accessory nerve. It’s defined by clonic spasms of the sternocleidomastoid muscle.
Clinical Testing of Spinal Accessory Nerve
Thesternocleidomastoid muscle is examined by asking the patient to turn his face to the reverse against the opposition given by the examiner’s hand. In a normal state, someone can do it and sternocleidomastoid stands out conspicuously. The trapezius muscle can be examined by asking the patient to shrug his shoulder against the resistance.


 (81 votes, average: 3.77 out of 5)
(81 votes, average: 3.77 out of 5)