Ovaries are those female organs which are the homologous of testes in the male. These can also be termed as female gonads. Their work is to generate female gametes termed as oocytes (mature ova). The ovaries are shaped like an almond and are grayish pink in color. Every ovary is all about 4 cm long, 2 cm wide and 1 cm thick.
Ovaries
Location
Ovaries: Location
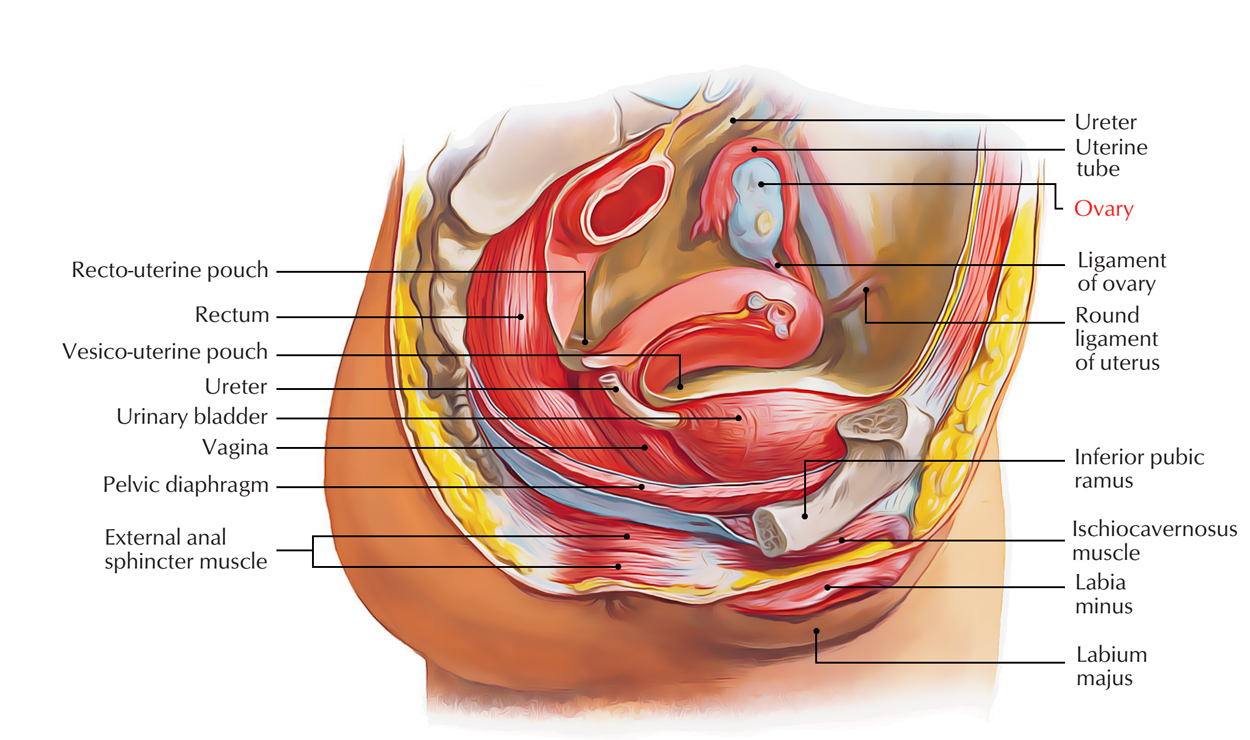
The ovaries are located in the ovarian fossa on the lateral pelvic wall below the pelvic brim in nulliparous adult women. A negligible peritoneal depression is the ovarian fossa which is also surrounded by:
- Posteriorly by the ureter and internal iliac vessels.
- Anteriorly by the external iliac vessels.
- Inferiorly by the uterine tubes (in the complimentary margin of broad ligament).
The obturator nerve and vessels cross the floor of the fossa.
Peritoneal Relationships
- Every ovary is connected to the posterior surface of the broad ligament by a short peritoneal fold termed mesovarium. Via mesovarium, ovarian vessels goes into the hilus of ovary.
- Every ovary is nearly completely covered by the peritoneum with the exception of along the mesovarian border where 2 layers of the covering peritoneum are reflected on the posterior layer of the broad ligament.
- The mesovarium functions as a hilum of the ovary and carries blood vessels and nerves to the ovary. The peritoneal layers of the mesovarium become constant with the germinalepithelium of the ovary. The junction between the flattened mesothelium of peritoneum and the cuboidal germinal epithelium of ovary is marked by white line of ovary (line of Furre).
External Features and Relationships
Ovaries: External Features and Relationships
Before the start of ovulation the surfaces of the ovary are smooth, but after puberty they get nodular. The external features of the ovary are constantly defined as observed in a nulliparous woman. In anatomical position, the long axis of the ovary is just about vertical so that it’s an upper post and a lower post. The ovary presents the following external features:
- 2 extremities or Poles.
- 2 surfaces.
- 2 edges.
In multiparous women (after 1 or more deliveries), the long axis of ovary becomes horizontal and its surfaces become uneven.
Extremities (or Poles)
Suspensory ligament of ovary.
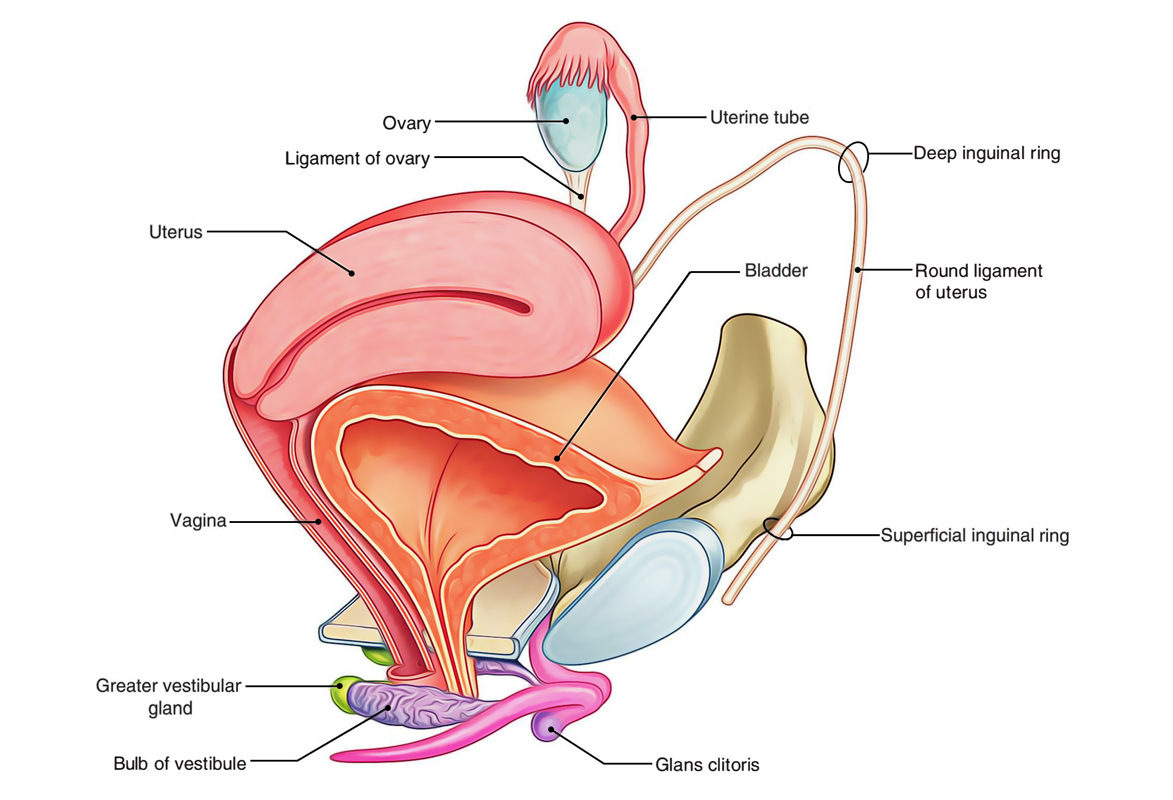
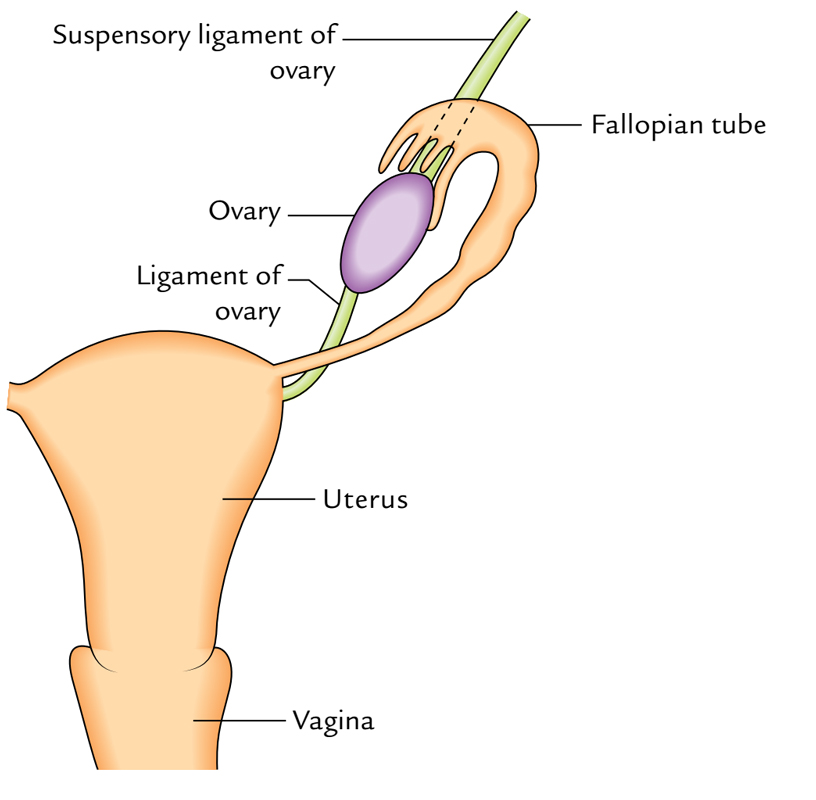
- Superior extremity: It’s wider than the lower extremity and is linked to the uterine tube and the external iliac vein. It gives connection to a fold of peritoneum named suspensory ligament of ovary which includes ovarian vessels and nerves.
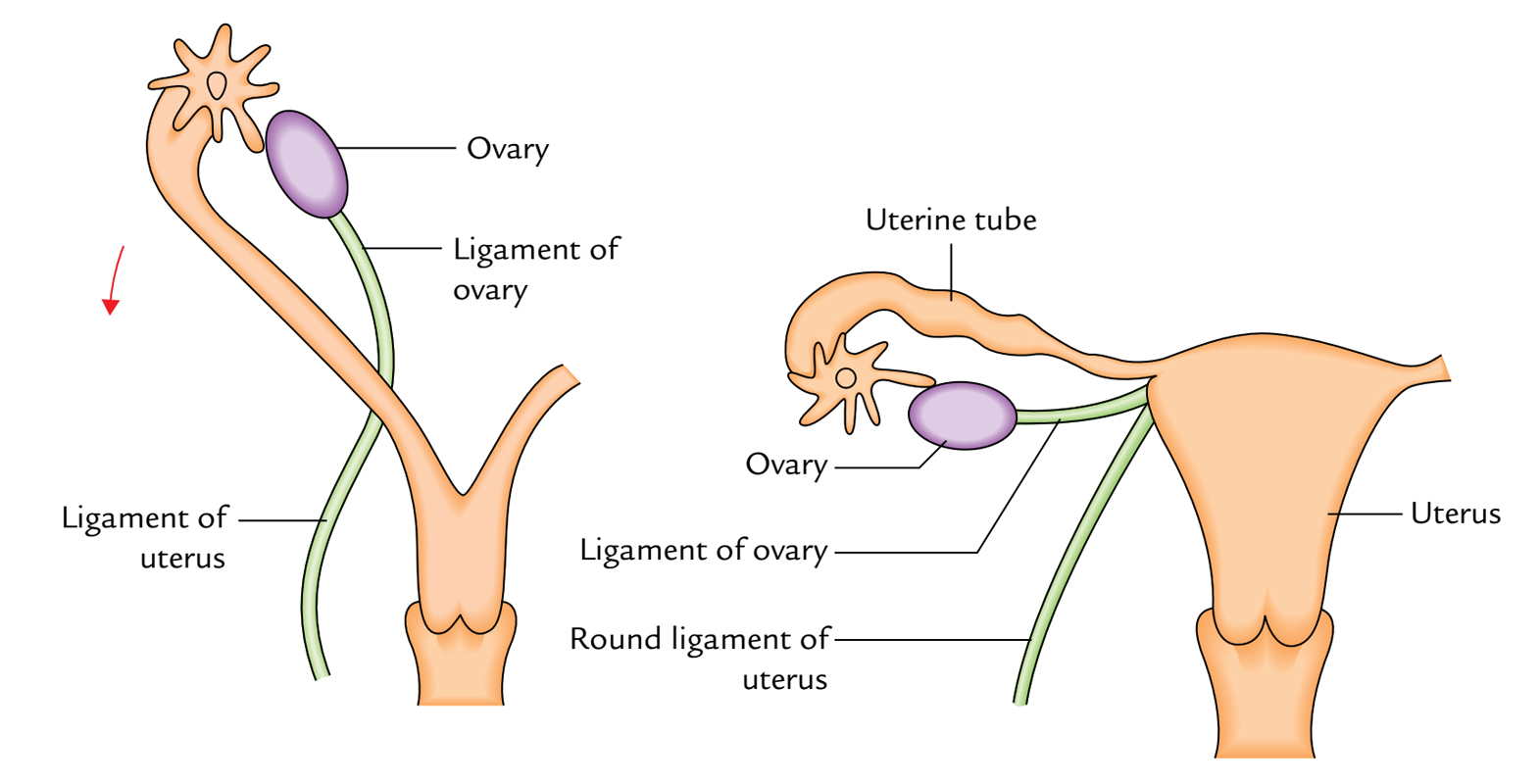
- Inferior extremity (orpole): It’s narrower in relation to the upper extremity and is linked to the pelvic diaphragm. It’s linked to the lateral angle of the uterus posteroinferior to the connection of fallopian tube by the ligament of ovary.
Surfaces
- Lateral surface: It’s convex and is in contact together with the parietal peritoneum lining the ovarian fossa. This surface splits the ovary from extraperitoneal tissue, and obturator nerve and vessels.
- Medial surface: To a large extent, this surface is covered by the uterine tube, from which it’s divided by a peritoneal recess termed ovarian bursa.
Borders
- Anterior (mesovarian) border: It’s straight and connected to the posterior layer of broad ligament by a brief fold of peritoneum named mesovarium.
- Posterior (free) border: It’s convex and is directed toward the uterine tube and is associated with the ureter.
Association of the ovary together with the fallopian tube: The uterine tube arches over the ovary running along its mesovarian border. It arch over its superior extremity subsequently enters downward on its free border and medial surface and makes direct contact with all the ovary by 1 of its fimbriae referred to as ovarian fimbria.
Structure
Ovaries: Structure
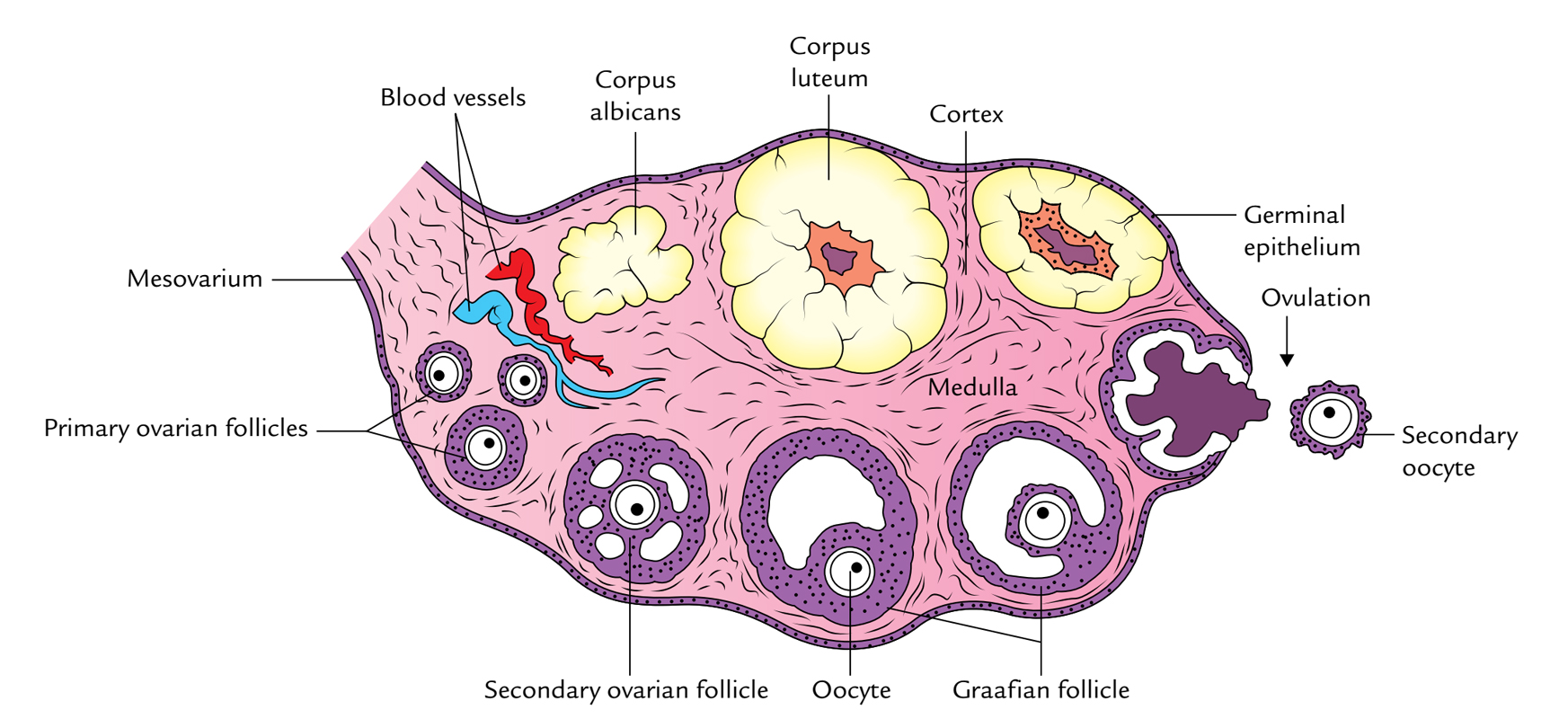
Cortex
The cortex is the thick peripheral part and includes ovarian follicles in distinct phases of adulthood.
It’s covered by the germinal epithelium that is created from a single layer of cuboidal cells in younger age. In the afterwards life, the epithelial cells become flattened. The germinal epithelium becomes constant with the peritoneum at the mesovarian border. Instantly underneath the germinal epithelium, the connective tissue of the cortex is condensed to create a whitish tough fibrous tissue layer named tunica albuginea.
Medulla
The medulla is located deep to the cortex. It is composed of loose connective tissue consisting of comparatively large blood vessels, especially veins.
Arterial Supply
Ovaries: Arterial Supply
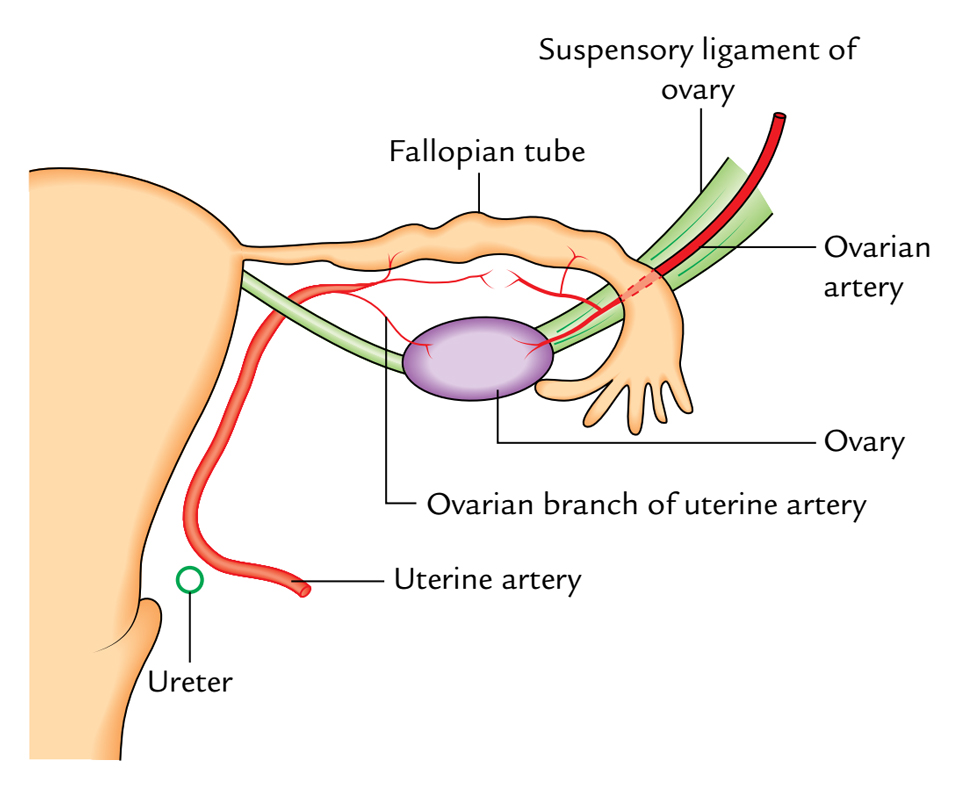
The ovary is primarily supplied by an ovarian artery which originates from the aorta in the level of L1 vertebra. It reaches the ovary after passing successively via the suspensory ligament of ovary, mesosalpinx, and mesovarium. It ends by anastomosing with the uterine artery. The ovary is also supplied by an ovarian branch of the uterine artery via the mesovarium.
Venous Drainage
The veins of the ovary come forth from the hilum and create the pampiniform plexus around the ovarian artery, from which a single ovarian vein is composed near the superior aperture of the pelvis/pelvic inlet. The right ovarian vein empties into the inferior vena cava while the left ovarian vein empties into the left renal vein.
Lymphatic Drainage
The lymphatics from the ovary follow the ovarian vein and drain into the pre-aortic and para-aortic lymph nodes (from the bifurcation of aorta to the level of renal vessels).
Nerve Supply
The ovary is innervated by the postganglionic sympathetic (T10, T11) and parasympathetic (S2, S3, S4) fibres, originated from abdominal autonomic plexuses. The function of autonomic nerves to the ovary is cloudy. In spite of the fact that normally it’s believed that sympathetic fibres are vasomotor and parasympathetic fibres are vasodilators.
The visceral afferent fibres from the ovary run along the sympathetic nerve pathways to the spinal sections T10, T11. The ovarian pain is sent in the umbilical region being supplied by T10 spinal section. The intractable ovarian pain can be relieved by transecting the suspensory ligament, which include the afferent (general visceral afferent) fibres.
The blood vessels, lymphatics, and nerves pass over the pelvic inlet, cross the external iliac vessels, and after that goes into the suspensory ligament of the ovary (lateral end of broad ligament) and eventually goes into the hilum of ovary via the mesovarium.
Clinical Significance
Ovarian Torsion
The torsion of an ovary may take place because of an abnormally long mesovarium and suspensory ligament of the ovary.
Prolapse of Ovaries
The ovaries are frequently prolapsed/ displaced into the pouch of Douglas where they can be palpated on per vaginal (PV) evaluation.
Ovarian Cyst
- One or more small ovarian cysts could be created because of the developmental arrest of the ovarian follicles.
- A large ovarian cyst with an encysted fluid could possibly be created from the corpus luteum of the pregnancy. It causes an anteroposterior bulging of the abdomen but doesn’t present shifting dullness. It ought to be discerned from ascsites which presents with shifting dullness.
Ovarian Carcinoma
The carcinoma of an ovary is common and accounts for about 15% of all cancers and 20% of gynecological cancers.
Teratoma
The ovary may occasionally include pluripotent cells, which may generate a teratoma.
Functions
The functions of the ovaries are as follows:
- Generation of oocytes (female gametes): During the reproductive life of females (30-45 years), ovaries create instead 1 mature ovum per menstrual cycle (of 28 days). The ovum develops into a small cystic follicle referred to as Graafian (ovarian) follicle, which ruptures roughly in the middle of menstrual cycle, i.e., 14th day, and discharges the ovum into the peritoneal cavity. After ovulation, the empty Graafian follicle is converted into a mass of specialized tissue named corpus luteum.
- Generation of hormones: The ovaries produce 2 hormones- progesterone and estrogen. The progesterone is secreted by the luteal cells and estrogen by the follicular cells.
Development
The ovary, 1 on every side, grows inside the abdominal cavity from a genital ridge on the posterior abdominal wall. The genital ridge is composed by the thickening of coelomic epithelium that covers the medial side of mesonephros. It gets primordial germ cells originated from the wall of the yolk sac.
Ovaries: Development
The ovary then descends into the pelvis. The descent includes the gubernaculum (a band of fibromuscular tissue) and processus vaginalis (a process of the peritoneum created because of its evagination).
The gubernaculum goes from the ovary to the junction of the uterus and uterine tube (creating the ovarian ligament in grownup) and after that continues in the labium majus (creating the round ligament of the uterus in the grownup). The processus vaginalis is obliterated in the adult.
Clinical Significance
Ovarian Dysgenesis
Congenital absence of 1 or both ovaries is seen in Turner’s syndrome.
Ectopic Ovaries
The ovary may fail to descend into the pelvis or very infrequently may be attracted downward with the round ligament of the uterus into the inguinal canal or even into the labium majus.

 (53 votes, average: 4.57 out of 5)
(53 votes, average: 4.57 out of 5)