In general language, the area between the anus and the genitals is known as the perineum. It can be found at the lower end of trunk and it is a noticeable diamond shaped area and can be noticed when the thighs are abducted and its margin is formed by the pelvic outlet.
Perineum
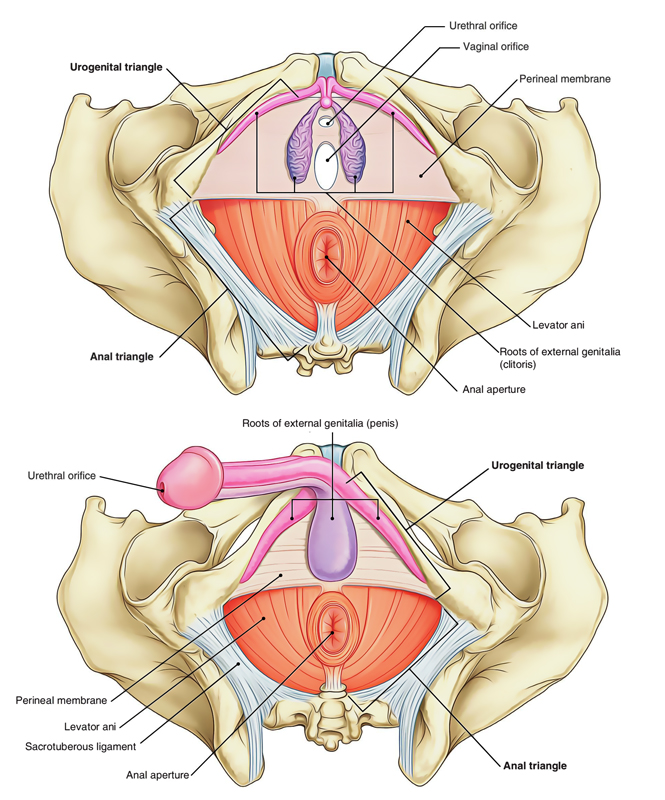
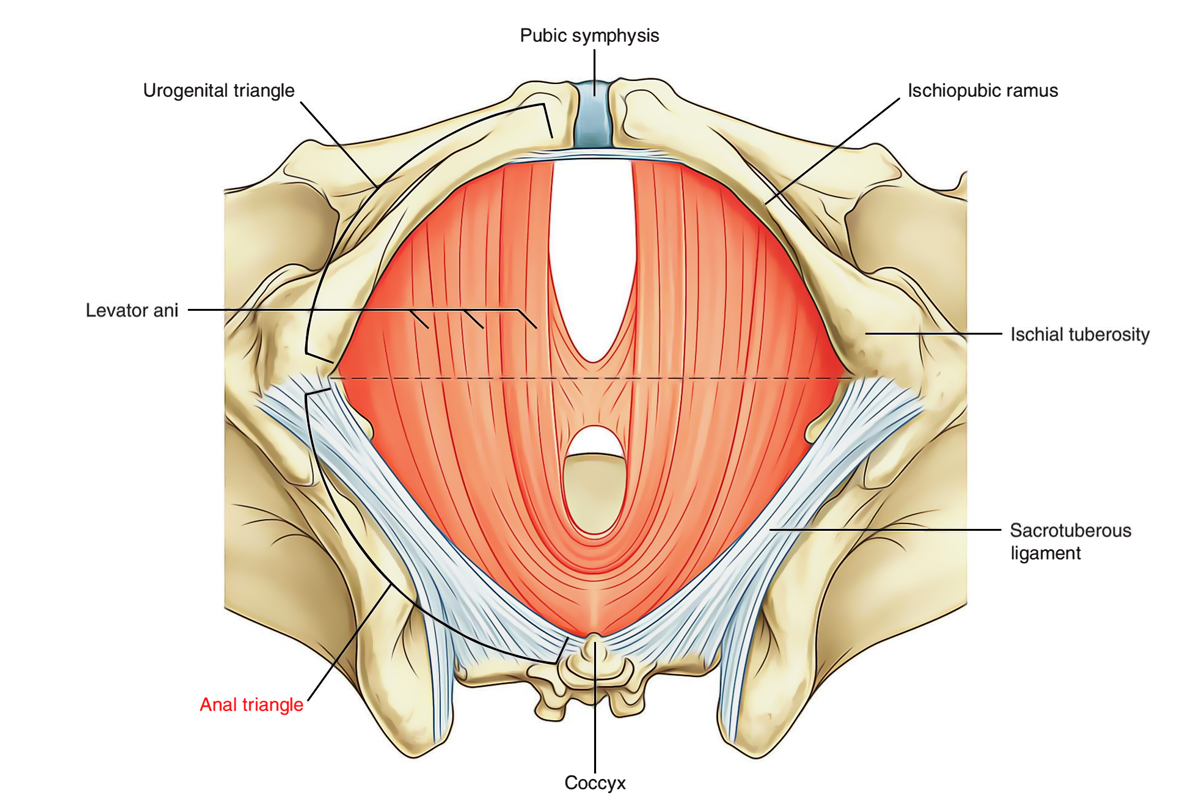
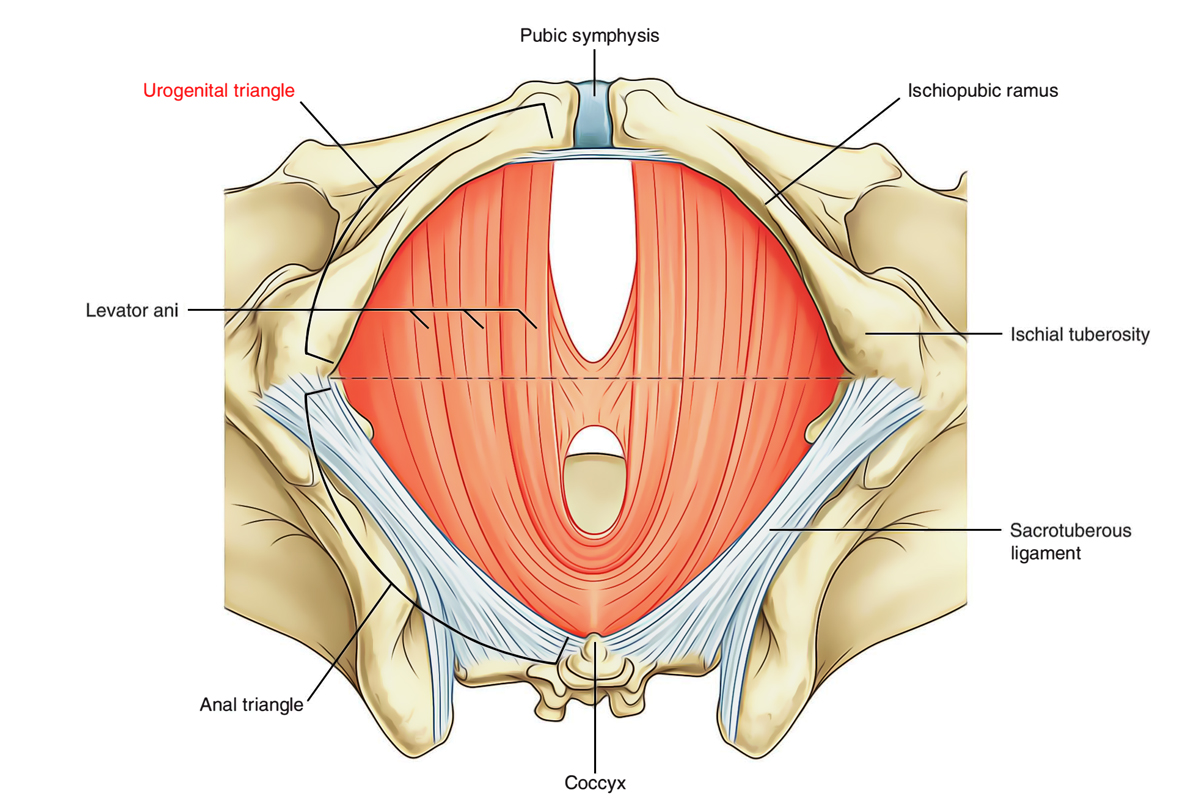
Perineum is divided into two triangular regions by an imaginary line between the ischial tuberosities.
- Anteriorly, the urogenital triangle of the perineum contains the roots of the external genitalia and, in women, the openings of the urethra and the vagina. In men, the distal part of the urethra is enclosed by erectile tissues and opens at the end of the penis.
- Posteriorly, the anal triangle of the perineum contains the anal aperture.
Borders
The perineum is an area summarized by the pelvic outlet. The borders and contents of the perineum are as follows:
The borders of perineum are:
- Anteriorly: Pubic symphysis.
- Posteriorly: Coccyx.
- Laterally: Ischiopubic rami (anteriorly) and sacrotuberous ligaments (posteriorly).
- The roof of perineum is composed by the pelvic diaphragm and its floor is composed by the skin.
Contents
Perineum forms a diamond shaped area. When viewed from below the perineum can be divided into an anterior urogenital region and a posterior anal region by a line joining the ischial tuberosities horizontally.
Anal Triangle
Perineum: Anal Triangle
The anal region of the perineum contains the anal canal and ischiorectal fossae.
• Anal canal: The anorectal junction is slung by the puborectalis component of the levator ani which pulls it forwards. The canal is approximately 4 cm long and angled postero-inferiorly. Developmentally, the midpoint of the anal canal is represented by the dentate line. This is the site at which the anal dimple in the skin, the ectodermal proctodeum, meets endoderm.
• Anal sphincter: Comprises external and internal components. The internal atiaf sphincter is a continuation of the inner circular smooth muscle of the rectum. The external anal sphincter is a skeletal muscular tube which, at its rectal end, blends with puborectalis to form an area of palpable thickening termed the anorectal ring. The competence of the latter is fundamental to anal continence.
• Ischiorectal fossae: Lie on either side of the anal canal. The medial and lateral walls of the ischiorectal fossa are the levator ani and anal canal and the obturator intemus, respectively. The fossae are filled with fat. The anococcygeal body separates the fossae posteriorly; however, infection in one fossa can spread anteriorly to the contralateral fossa forming a horseshoe abscess. The pudendal (Alcock’s) canal is a sheath in the lateral wall of the ischiorectal fossa. It conveys the pudendal nerve and internal pudendal vessels from the lesser sciatic notch to the deep perineal pouch (see below). The inferior rectal branches
of the pudendal nerve and internal pudendal vessels course transversely across the fossa to reach the anus.
| Muscles | Origin | Insertion | Innervation | Function |
|---|---|---|---|---|
| EXTERNAL ANAL SPHINCTER | ||||
| Deep part | Surrounds superior aspect of anal canal | Pudendal nerve (52 and 53) and branches directly from 54 | Closes anal canal | |
| Superfcial part | Surrounds lower part of anal canal | Anchored to perineal body and anococcygeal body | ||
| Subcutaneous part | Surrounds anal aperture | |||
Urogenital Triangle
Perineum: Urogenital Triangle
The urogenital triangle of the perineum is the anterior half of the perineum and is oriented in the horizontal plane. The urogenital region is triangular in shape. It is composed of the roots of the external genitalia and the openings of the urogenital system.
The urogenital triangle of the perineum is defined as:
- Laterally by the ischiopubic rami.
- Posteriorly by an imaginary line between the ischial tuberosities.
- Anteriorly by the inferior margin of the pubic symphysis.
As with the anal triangle, the roof or ceiling of the urogenital triangle is the levator ani muscle. Unlike the anal triangle, the urogenital triangle contains a strong fibromuscular support platform, the perineal membrane and deep perineal pouch, which is attached to the pubic arch. Anterior extensions of the ischio-anal fossae occur between the deep perineal pouch and the levator ani muscle on each side.
Between the perineal membrane and the membranous layer of superfcial fascia is the superfcial perineal pouch. The principal structures in this pouch are the erectile tissues of the penis and clitoris and associated skeletal muscles.
There are five layers of the urogenital triangle namely:
Deep Perineal Pouch: A space between deep fascia of the pelvic floor and perineal membrane.
Perineal Membrane: A tough solid layer penetrated by the urethra.
Superficial Perineal Pouch: A considerable space between perineal membrane and superficial perineal fascia.
Perineal Fascia: It is the continuation of abdominal fascia which consists of two components namely: deep and superficial fascia.
Skin: The urethral and vaginal orifices that opens out on to the skin.
Structures in the Superfcial Perineal Pouch
The superfcial perineal pouch contains:
- Srectile structures that join together to form the penis in men and the clitoris in women, and
- Skeletal muscles that are associated mainly with parts of the erectile structures attached to the perineal membrane and adjacent bone.
Each erectile structure consists of a central core of expandable vascular tissue and its surrounding connective tissue capsule.
The perineal membrane is a strong fascial layer that is attached to the sides of the urogenital triangle. In the male, it is pierced by the urethra and, in females, by the urethra and vagina.
In the female
Vulva
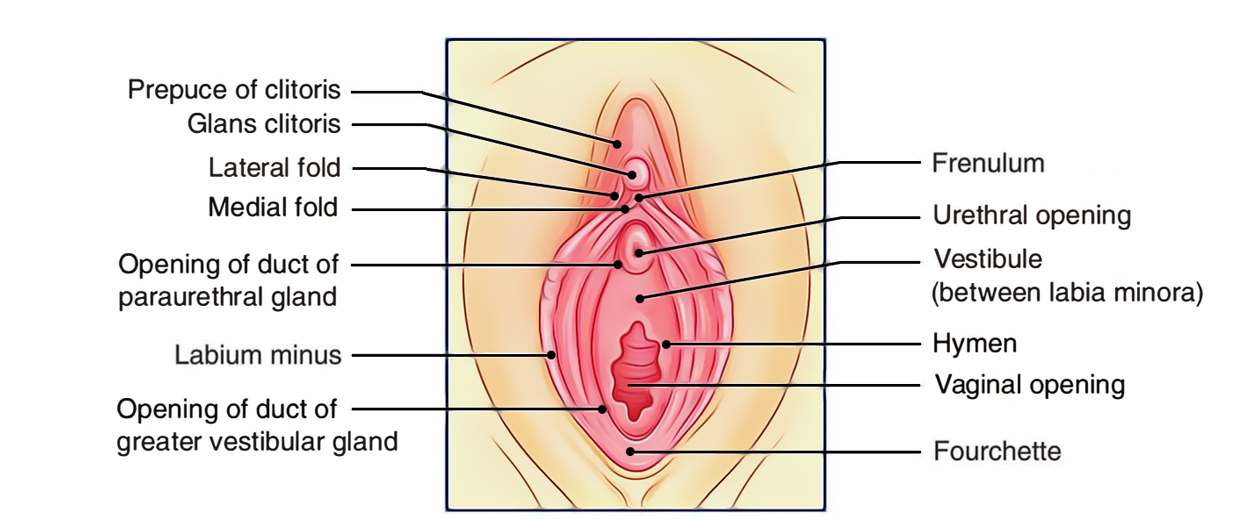
Vulva is the term given to the female external genitalia. The mons pubis is the fatty protuberance overlying the pubic symphysis and pubic bones. The labia majora are fatty hair-bearing lips that extend posteriorly from the mons. The labia minora lie internal to the labia majora and unite posteriorly at the fourchette.
Anteriorly, the labia minora form the prepuce and split to enclose the clitoris. The clitoris corresponds to the penis in the male. It has a similar structure in that it is made up of three masses of erectile tissue: the bulb (corresponding to the penile bulb) and right and left crura covered by similar but smaller muscles than those in the male. As in the male, these form the contents of the superficial perineal pouch. The deep perineal pouch, however, contains the vagina as well as part of the urethra, sphincter urethrae and internal pudendal vessels.
The vestibule is the area enclosed by the labia minora, which contains the urethral and vaginal orifices. Deep to the posterior aspect of the labia majoris lie Bartholin’s glands (a pair of mucus-secreting glands that drain anteriorly0. They are not palpable in health but can become grossly inflamed when infected.
Urethra
Urethra is short in the female (3-4 cm). It contributes to a relative predisposition to urinary tract infection in females from an upward spread of bowel organisms. The urethra extends from the bladder neck to the external meatus. The meatus lies between the clitoris and vagina.
Vagina
Perineum: Vagina
Vagina measures approximately 8-12 cm in length. It is a muscular tube that passes upwards and backwards from the vaginal orifice. The cervix projects into the upper anterior aspect of the vagina creating fornices anteriorly, posteriorly and laterally. Lymph from the upper vagina drains into the internal and external iliac nodes. Lymph from the lower vagina drains to the superficial inguinal nodes. The blood supply to the vagina is from the vaginal artery (branch of the internal iliac artery) and the vaginal branch of the uterine artery.
In the male
The external urethral sphincter (striated muscle) lies deep to the perineal membrane within a fascial capsule termed the deep perineal pouch. In addition to the sphincter, two glands of Cowper are also contained within the deep pouch. The ducts from these glands pass forwards to drain into the bulbous urethra. Inferior to the perineal membrane is the superficial perineal pouch, which contains the:
- Superficial transverse perineal muscles: run from the perineal body to the ischial ramus.
- Bulbospongiosus muscle: covers the corpus spongiosum.
The latter structure covers the spongy urethra.
- Ischiocavernosus muscle: arises on each side from the ischial ramus to cover the corpus cavernosum.
It is the engorgement of venous sinuses within these cavernosa that generates and maintains an erection.
Hence, the penile root comprises a well-vascularised bulb and two crura which are supplied by branches of the internal pudendal artery. The erectile penile tissue is enclosed within a tubular fascial sheath. At the distal end of the penis the corpus spongiosum expands to form the glans penis. On the tip of the glans, the urethra opens as the external urethral meatus. The foreskin is attached to the glans below the meatus by a fold of skin – the frenulum.
The Scrotum
The skin of the scrotum is thin, rugose and contains many sebaceous glands. A longitudinal median raphe is visible in the midline. Beneath the skin lies a thin layer of involuntary dartos muscle. The terminal spermatic cords, the testes and their epididymides are contained within the scrotum.
Testis and Epididymis
The testes are responsible for spermatogenesis. Their descent to an extra-abdominal position favours optimal spermatogenesis as the ambient scrotal temperature is approximately 3°C lower than the body temperature.
Structure: the testis is divided internally by a series of septa into approximately 200 lobules. Each lobule contains 1-3 seminiferous tubules, which anastomose into a plexus termed the rete testis. Each tubule is coiled when in situ, but when extended measures approximately 60 cm. Efferent ducts connect the rete testis to the epididymal head. They serve to transmit sperm from the testicle to the epididymis.
- The tunica vaginalis, derived from the peritoneum, is a double covering into which the testis is invaginated.
- The tunica albuginea is a tough fibrous capsule that covers the testis.
- The epididymis lies along the posterolateral and superior borders of the testicle. The tunica vaginalis covers the epididymis with the exception of the posterior border.
- The upper poles of both the testis and epididymis bear an appendix testis and appendix epididymis (hydatid of Morgagni), respectively.
Blood supply: is from the testicular artery. Venous drainage from the testicle is to the pampiniform plexus of veins. The latter plexus lies within the spermatic cord, but coalesces to form a single vein at the internal ring. The left testicular vein drains to the left renal vein, whereas the right testicular vein drains directly to the inferior vena cava.
- Lymphatic drainage: is to the para-aortic lymph nodes.
- Nerve supply: is from T10 sympathetic fibres via the renal and aortic plexuses.
Perineal Body
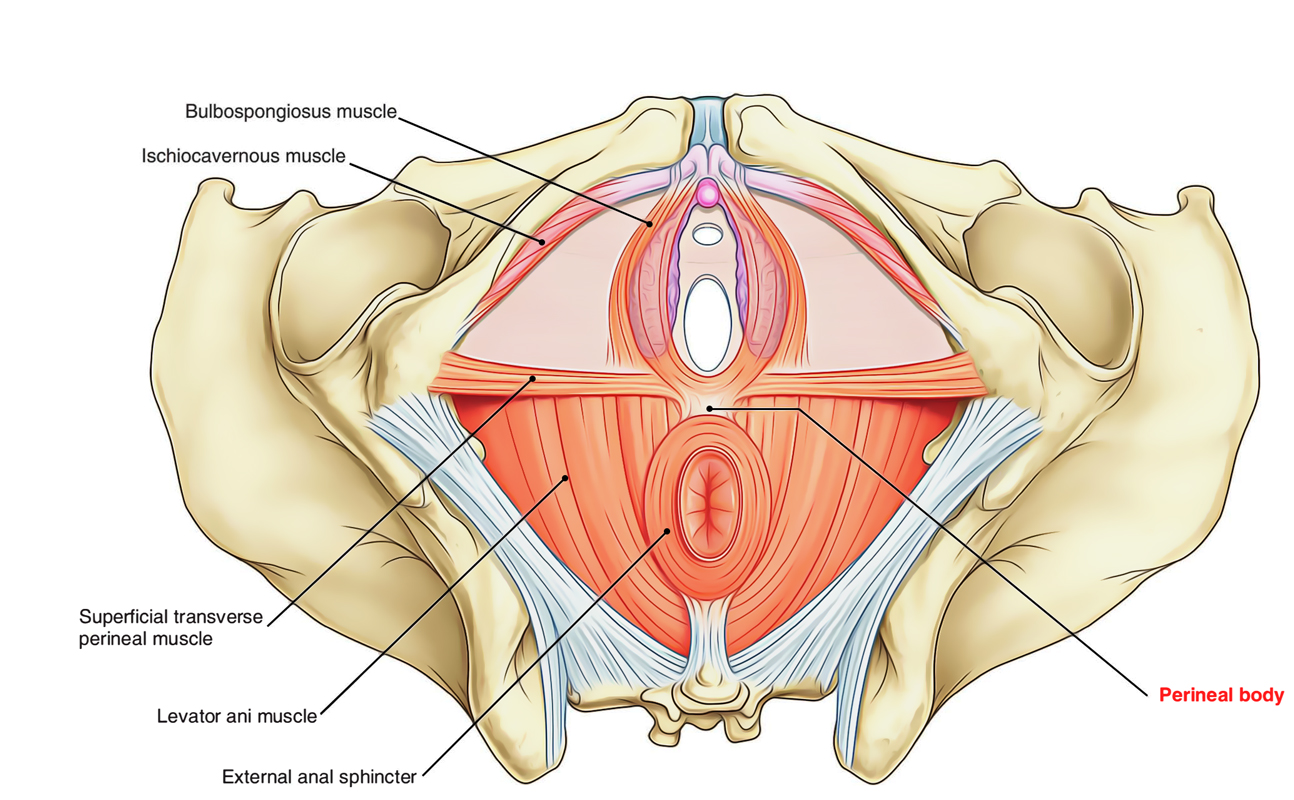
Perineum: Perineal Body
The perineal body is a pyramidal fibromuscular node situated in the midline in the angle between the anal canal and the urogenital apparatus. In female it is also called obstetric perineum or gynecological perineum.
Situation
About 1.25 cm in front of anal margin and close to the penis.
Muscles Attached to Perineal Body
Anatomically, the perineal body lies deep to the skin. It plays a crucial role acting as an attachment for muscle fibres originating from the pelvic floor and the perineum itself:
1. Three paired muscles:
- Transversus perinei superficialis
- Transversus perinei profundus
- Levator ani (one of the parts of the pelvic floor)
2. Three unpaired muscles:
- Sphincter ani externus
- Bulbus spongiosus
- Longitudinal muscle coat of rectal ampulla.
Functions
It is very important in females for the support of the pelvic organs.
Clinical Significance
1. Perineum’s involvement or tearing may occur during spontaneous delivery produce prolapse of the following:
- Urinary bladder
- Uterus
- Ovaries
- Rectum
- Vagina.
2. As perineum is the final support of the pelvic visceras therefore, its tearing may result permanent weakness of the pelvic diaphragm.
3. Perineal body can also be disrupting by trauma, inflammatory disease and infection which may produce fistula that connected to the vestibule of the vagina.
The Importance of the Perineum in Childbirth
While giving brith to a child, the perineum expands enormously for facilitating the mother to push the baby out. Sometimes this forces perineum to tear, which is really difficult to repair by stitching and it also might take a good amount of time to heal.
The risks of a tear are higher during the first vaginal birth especially in case of a large baby, if there’s a substantial weight gain during pregnancy, or maybe you are either younger or older.
While obsreving the pregnancy period, regular perineum massages can facilitate to stretch the perineum and avoid tears to occur. This is also referred to as birth canal widening, perineum stretching can be done at home during the final weeks leading up to your due date.
The main aim is to master the skill of relaxing your pelvic floor muscles and expand the vaginal opening. Your obstetrician or midwife can show you how to give a perineal massage.
Common causes of perineum injuries
- Falling on a crossbar of a cycle or a bike.
- Intense sex routine.
- Getting hurt in the groin while playing a sport.
- Climbing activities.
Injured perineum can also hinder your sex if the nerves and blood vessels in the perineum get damaged.
Test Your Knowledge
Perineum

 (53 votes, average: 4.53 out of 5)
(53 votes, average: 4.53 out of 5)